To call the past twelve months chaotic would be the understatement of the millennia. Faced with a once-in-a-century pandemic that was uniquely infectious and deadly, billions around the world fundamentally altered their lives with the hopes of slowing the spread of the illness. It can be hard to think of a past event that completely changed people’s lives.
This is the story of how it could end. How after month after month of this global nightmare, we may emerge damaged, but alive. How the virus left some of us with severe and potentially lifelong scars, and others remained untouched. And most importantly how a return to normalcy may look.
“The lack of being able to meet up with the friends and family I love and care for has made me realize the weight they hold in my happiness,” junior Daman Sandhu said. “This has all definitely been a learning experience.”
A Shot in the Dark
One of today’s questions is whether or not to take the COVID-19 vaccine. Most Americans are looking for answers on social media, television, and the internet. There’s so much information – both false and true – that it’s hard for many to feel like they are making the “right” decision. Not to mention the overwhelming amount of emotions involved, be it fear of possible side effects or eagerness to feel safe.
For many, personal experiences and the loss of loved ones has helped them make their decision. People have developed or experienced negative increases in mental illnesses and disorders, lost their jobs and possibly their loved ones. Situations such as these pushed people like Dr. Cynthia Wong, respiratory teacher, to take the vaccine.
“When the vaccine was being developed, I was on the fence about taking it, but then two of my family members passed away from COVID-19 over the holidays,” Wong said. “So, it got real for me really fast. They were healthy and walking around, and they said they had allergies. [Within a few] days, we went to the hospital and they never came out. After that, I thought that it was pretty serious. I have a lot of faith in science, so I think it will be okay. I want to help myself out.”
Wong was one of the few who decided to take the vaccine sooner than later, receiving the vaccine a little more than a month after the first shipment of COVID-19 vaccinations arrived in Southern Nevada.
“I took the Pfizer vaccine. I didn’t have the choice, but I don’t really care. It wasn’t a bad experience at all,” Wong said. “I barely even felt the shot. A lot of people say the arm is really sore afterwards, but it’s just a little soreness. The bruising comes a little later, but the actual injection area isn’t really sore.”
Besides the possible side effects, the distribution of the vaccines is a deciding factor. America is already behind on the vaccine rollout plan, with 76.9 million vaccines administered across the country and 723,000 in Nevada. Wong’s relatives are part of the many who haven’t received the vaccine.
“My parents are in California, and they are in their eighties and they still can’t get the vaccine,” Wong said. “So, it’s kind of ridiculous. We are so lucky that here in Las Vegas we can get it. I don’t know what’s happening in California, but I think that if they’re 75 years old or older then they should just be handing out vaccinations. I know the primary care doctors over there don’t have it yet. The pharmacies don’t have it yet. So I don’t know who’s getting vaccinated in California, but it’s not the elderly.”
One problem with the delayed vaccine rollout is that former President Donald Trump’s strategy was to reserve some vaccines to ensure that those who received their first dose would get a second. It was later discovered that the Trump administration had no vaccines in reserve. President Joe Biden is taking a different approach and distributing all vaccines as they are produced.
The government is furthering its efforts to increase the vaccine rollout by increasing the supply of weekly vaccine doses to 11 million and increasing supply by 5% each week. Additionally, the government is launching a program to ensure that the vaccines are distributed equitably. They will directly ship doses to federally qualified community health centers where two-thirds of patients served have annual incomes at or below the federal poverty level, and 60% identify as ethnic or racial minorities.
Despite the vaccines’ availability, some are still against it, like Bophan Leng, a nurse at St. Rose Dominican Hospital. Due to her personal beliefs, she decided it would be best not to get vaccinated.
“I’m a Buddhist and Christian,” Leng said. “I believe putting something foreign into my body is not appropriate. I can regulate my body better without something being put inside it. I’m sure that I’m pretty healthy. I don’t drink. I don’t smoke. I kind of regulate what I intake. I believe that my body will eventually work its way towards getting stronger.”
Although America is doing better than the vast majority of our allies with regard to vaccination allocations, there are still setbacks. Many states just aren’t administering the doses shipped to them. Some states don’t have the infrastructure to manage the volume. For example, Miami-Dade County released 2,000 appointments, and they were gone in under a minute as 80,000 people slammed the reservation site.
Many counties without staff and structure failed to account for the demand. Vaccines are accidentally being discarded. A single vial of the Pfizer vaccine contains five doses. Once a vial is opened, it must be used within six hours. In a situation where someone misses their appointment or changes their mind, the vaccines are wasted.
In one of the many counties of Houston, Dr. Hasan Gokal was fired for stealing a vial of the COVID-19 vaccine from a Harris County Public Health District distribution site last year.
“In the event you get leftover with any vaccine, don’t waste any,” Gokal said during an interview in February. “Go find people who are eligible in that tier. If you can’t find any, go to the next tier. If you can’t find that, give it to anybody who’s willing and able to take it. As far as throwing away the doses versus giving them away to the people who deserved them, I think I wouldn’t be a good physician if I said I regretted doing that.”
Most experts believe the pandemic is going to end if the country achieves herd immunity. The US has vaccines that will help protect people against COVID-19, and researchers estimate that about 60 to 70% of the population must be vaccinated. After seeing the data, some people think the US will achieve herd immunity by the beginning of 2022. Although the statistics lead Americans to believe that the nation will reach herd immunity, some people are still not convinced. About 15% of Americans say that they don’t intend to get vaccinated. The problem with reaching herd immunity is that the percentage of transmission must be lowered, however, some variants of the coronaviruses are more easily transmissible.
“I don’t believe that we will get to herd immunity,” Leng said. “The virus is still mutating, so scientists and doctors would have to come up with a vaccine that could fight against all strains, but we don’t have that. Personally, I feel like we’re going to live with this virus the same way we have with the flu. I haven’t taken the flu shot, and I haven’t gotten the flu. I pretty much keep a healthy regiment. So people will be able to live with this virus, but I don’t believe everyone will be able to live without getting COVID-19.”
Despite her beliefs about the vaccine, she still respects other people’s decisions and looks after her children’s safety.
“I vaccinated my kids because they’re younger, and their immunity isn’t as strong,” Leng said. “As for my patients, it’s really up to them. I try to educate them on all that nurses have been taught about the vaccine, and I don’t force them to choose one thing or another. I don’t like that the media is trying to do that, because really it’s up to the individual. People have their own choice. I think this country is best when freedoms can be expressed. This vaccine shouldn’t be forced upon anyone.”
Every choice Americans make today will count towards what the next few years will look like, whether it be another lockdown or the freedom and comfort in traveling out of state without the concern of being infected. People who were not affected should inform themselves before choosing to take the vaccine.
“Everyone is different, and the vaccine isn’t mandatory at this point,” Wong said. “But just looking at the numbers, that’s almost like half a million people that have passed from COVID-19. I don’t like those odds, and I had people close to me who have passed from it. Before that, I would hear that a friend of a friend of a friend had got it, and now it’s getting way too close. So it was important for me to look at all the information and make a smart decision, which for me it was like, ‘I should just get the vaccine!’ All the information pointed that way.”
A new virus saga?
Throughout human history, viruses and bacteria have adopted the obnoxious habit of mutating to better fit their environments. These mutations cause changes in their DNA, initiating potentially dangerous symptoms.
Lately, variants from the United Kingdom, Africa, and South America have sparked a new fear of a second wave of the fatal COVID-19 virus. Questions have arisen among the American population, such as whether these variants are more fatal or contagious, or if they will affect the current response for COVID-19 so far.
These variants differ from each other due to their spike proteins. These spike proteins allow the virus to invade and infect human body cells. However, viruses mutate to escape the immune system easier. As seen in the influenza virus, genes change over time to allow mutated genes to defeat the immune system easier, do their job, and become the dominant strain until a new and stronger mutation occurs.
In an interview with Dr. Puri Pascual in February, a doctor in California (one of the first states to detect the new U.K. variant), Pascual said there is no clear information on the new variants right now.
“Although there are some reports that it can be spread easily and quickly, we can study and certainly identify whether this can force a more severe response, leading to more hospitalization,” Pascual said. “It will definitely put a strain on our healthcare system if there’s an outbreak. Hopefully, with the goal of vaccinating 80% of the population, this will lead to the decline of the variants.”
Although Pascual sees potential in the fight against the new variant with the vaccines, Dr. Raoul Tamayo, a resident doctor in Las Vegas, says the new strains present a potent set of problems.
“The variant one is actually pretty deadly as well. We’re not protecting ourselves properly with social distancing, proper handwashing, and wearing masks,” Tamayo said during an interview in late January. “Luckily, if we didn’t close our borders or limit people coming into the U.S., we would’ve been in more trouble in the next couple of months.
Additionally, Tamayo says the variants won’t stop since the virus continually mutates. Four thousand variants exist in the world today, which may pose an endless pandemic in the future.
“They’re smarter than us, the virus is pretty smart. They know they’re going to be killed, so they change their form,” Tamayo said. “It’s like the flu; we get to guess what kind of flu variant it is. That’s how we figure out what vaccine we’re going to give that year.”
Along with vaccines, Pascual also addressed the problem of using oxygen for treatment. A more contagious variant could mean more severe intubations.
“Some patients have different spectrums of severity. Lately, I’ve seen more and more young adults been affected with this, and once they are in high-flow oxygen, it’s really hard to wean them off of a specific oxygen level,” Pascual said.
Fortunately, Tamayo says that the current vaccines may combat the strains with some modification, known as booster shots.
“They haven’t really had any studies on this as long, but today Moderna says their vaccine is effective against these strains,” Tamayo said. “Even people who had prior infection probably can get infected more easily, but the 95 percent effectiveness on the original strain should work on this one.”
Worse still, another deadlier wave will affect both our overworked healthcare workers and the economy. This risk is amplified by the quick reopening of states, like Texas and Mississippi. Dino Avellaneda, a nurse at Desert Springs Hospital, says he still has hope that the already-full hospitals can take one more hit.
“In the first wave, we were flooded with so many patients and deaths in the hospital. In my opinion, it’s not going to be worse since we have the vaccine done,” Avellaneda said. “I think we’re doing okay vaccine-wise. We have to be optimistic about it.”
However, healthcare workers fear further infection and hardships due to new strains. They fear for themselves, their families, and their patients.
“I don’t want to be exposed, I don’t want to get sick. Worst thing happens, you’re on the machine. COVID is death,” Avellaneda said. “It’s hard when you’re taking care of three patients at the same time with COVID. I feel like I’m not able to do my job as a nurse, taking care of all these people. You want to take care of them, but you have no help.”
Right now, there is no easy solution to solve this unpredictable situation. These new variants are worthy of concern regarding a second, deadlier wave. The most provocative solution is to implement a new wave of shutdowns, despite the expected damage.
“I would shut everything down right now. I would have no foreign travels in the U.S. Only essential workers, hospital workers, people delivering food to be open,” Tamayo said. “Everything closed, we should probably do what Australia did. Trace and find the source, having proper systems, etc.”
Tightening restrictions
Like billions of people last summer, junior Kyle Peng planned on a nice vacation in a foreign country after a tumultuous point in this life. Amid a work-heavy sophomore year, the aspiring chef made plans to travel to Singapore with his family. He would enjoy the relaxing stay in a country known for its authentic dishes and unique Asian culture.
And then the coronavirus hit.
“I felt really sad because we usually go on a trip every year,” Peng said. “Singapore has a mix of a bunch of Asian cultures and creates beautiful dishes.”
Peng is far from the only person whose plans were cancelled due to COVID-19. The pandemic, and the travel restrictions that followed, have undermined millions of Americans’ plans. Fearing an overwhelming rise in the hospital systems, public officials in the state, country, and worldwide justified lockdowns as a necessary step in slowing the spread of COVID-19 – a step that included the shutdown of almost as travel. While there’s a lot of talk over the kinds of restrictions that may be lifted as America approaches herd immunity, travel restrictions appear just as likely to tighten.
Restrictions began lightly relative to the ones that came after then-President Trump curbed travel from China days after the first cases in America were detected. As COVID-19 spread across the globe, travel restrictions were increasingly implemented and tightened in an attempt to contain the virus. Now, these limitations are common, especially in areas heavily impacted by the pandemic.
Countries across the EU, some of whom have been ravaged by the pandemic more than the U.S. has, are far from keen on lifting them any time soon, even with a new vaccine. While some of this is due to the new and ominous strain variations of the virus that have sprung up from the UK and South Africa, countries’, hesitance to eliminate travel restrictions is mainly because of the mounting number of cases.
“With more people coming in from different places and on top of that, those people possibly in contact with the virus, it will definitely be risky and dangerous for me to go out,” junior Michelle Nguyen said.
These restrictions attracted much attention and debate as a means of combating the virus. Trump touted his early travel ban on China as a massive success, while fact-checkers and now-President Joe Biden pointed out that nearly 40 thousand people flew to the U.S. from China. Questions about how effective travel restrictions were in slowing the spread of the virus arose as more countries implemented them. Though some scientists argue that the effects of travel restrictions are overstated, the academic consensus seems to be on the side that travel restrictions were effective.
“If there aren’t any restrictions to traveling, this causes an increase of COVID-19,” microbiologist at Sunrise Hospital Carol Batara said.
As the political clashes over school reopenings come to an end in the upcoming months, many people are expected to return to in-person learning. Unfortunately for some students, it appears as though they’ll be learning about the mitochondria in-person before they get to enjoy seeing family outside Nevada.
But for many, the worst effect of these restrictions were social – the inability to travel outside their homes to attend the conventions, parties, and get-togethers they normally would. This social stasis has had adverse consequences on people’s mental health. Some people believe both that restrictions were necessary and that they’ve had a personally negative effect.
“I was devastated when COVID-19 started because of the things I knew I was losing, [like] having the opportunity to see my friends and extended family,” junior Lilley Mearns said. “I’m super family-oriented, and I have been surrounded my family my whole life, so it was definitely a huge change when we became distant because of guidelines.”
What “getting back to normal” looks like remains an open question. But for some, it’s as simple as just being able to do the things we were able to do before March of 2020.
“Being locked inside is really tough,” junior Chase Barranco said. I’m really upset that I had a year of my social life stolen from me.”
What will the classroom look like?
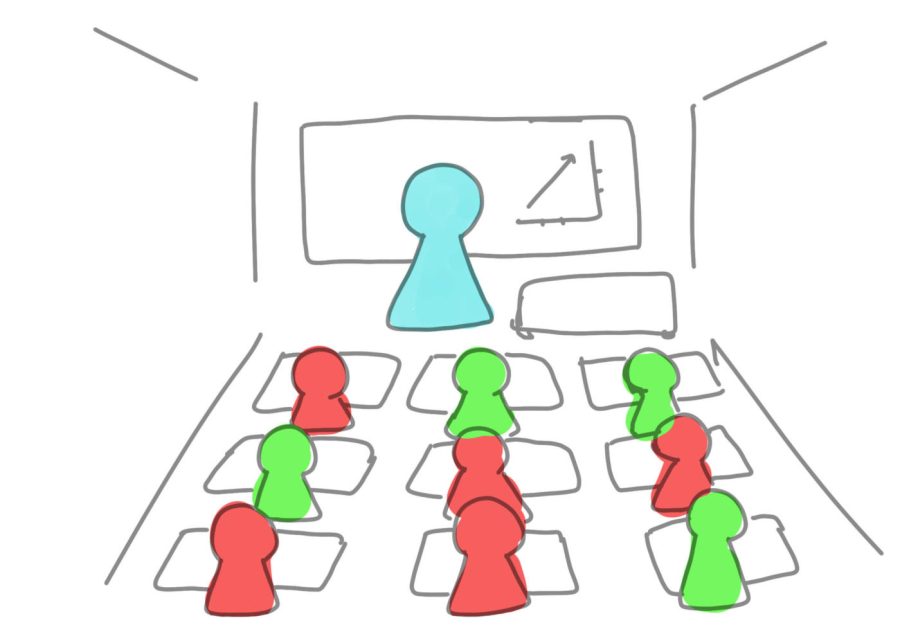
It’s been more than 365 days since the start of distance learning for schools across the country. Questions of how and when students will return have dogged school board members. Those questions have since been answered after CCSD announced on Feb. 24 that students will begin transitioning back to face-to-face instruction under a hybrid model plan.
As of March 1, students in Pre-K to third grade have returned to face-to-face instruction, and they will be followed by other grades throughout the month and into April. The hybrid model will consist of three cohorts: one will have students stay online throughout the week, while the other two will have students go in-person for two days and two days online.
There have been mixed reactions to the hybrid model. One of the people in disagreement with the plan is English 9 teacher Jessica Wolfenden, who has two elementary school children: a kindergartener and a second-grader.
“I was hopeful [about the hybrid plan] at first until I got all the information that it’s not going to be like school,” Wolfenden said. “I didn’t feel like it was the best option. I feel like it’s now this late in the game and it’s going to cause disruption. I feel like some of the kids, or at least my kids, will be missing out on some of the vital instruction that they’re definitely going to need moving forward. That they could’ve better obtained if we just stayed distant.”
For high schools in CCSD, in-person learning for some cohorts begins on March 22. Students have received emails that discussed what the model looks like, such as the three types of cohorts and what students will do on campus. Though CCSD has provided a comprehensive review of their policies for in-person learning, such as regulating traffic patterns and limiting the number of people in the restroom, some students have chosen to remain virtual.
“I personally chose Cohort C because it’s easier on my family and myself,” junior Akizcha Unating said. “My parents go to work during these hard times, so the least I can do is watch my little brother while I’m at school.”
After hearing about the hybrid learning plan, Unating had questions about how the cohorts would work and how long each class would take. Asides from not wanting to add burden onto herself and her family, she, ultimately, would rather not go back in-person.
“I think we should’ve stayed online for the last quarter of the year,” Unating said. “I understand seniors want to have their full high school experience, but you won’t get that if you come back. But I understand people aren’t mentally in the right mindset with this online learning so I think having the option to go back for some students is really good even if it’s only for a few hours. I just think the planning was a bit rushed and sloppy.”
Amongst the discussion is the COVID-19 vaccine and how it will affect school plans. Currently, children younger than 16 can’t receive the vaccine, and residents 65 or older will be the next group to receive them. Even if elementary school teachers have received it when schools open back, the students are potential carriers of the virus, and they can pass it on to people in their homes, or to their peers and teaching in the classroom.
For high school students, some of them between the ages of 16 to 18 will be allowed to receive the vaccine. SWCTA principal Donna Levy has hope that it’ll help students if they choose to return face-to-face.
“Hopefully, a lot of our students who turned 16 will get the opportunity to get it [vaccine],” Levy said. “If they all get it, we can get back to doing what we do, which is a lot more fun than what we’re doing now. And hopefully enough people will have it so we’d have herd immunity. I’m very excited.”
Even with the hope that the plans for face-to-face and hybrid will work out for students, teachers, and staff throughout the district, for now, they will have to adjust to their new environments.
“I do think that the mental health of these kids is super important, and I want things to go back to normal, just like everyone else,” second-grade teacher Angela Deer said. “But I also think that going back in the classroom isn’t going to be normal, unfortunately at this time. Even in a hybrid model, the kids sitting in desks 6-feet apart, we can’t take them to the lunchroom to eat lunch with their friends, and they’re sitting stationary for long periods of time. You know, for 7-year olds, that’s asking a lot. I think my kids are pretty resilient, so they could totally take me by surprise and blow me away and just handle things fine.”
Closing this chapter
With new strains being a thorn in the side of reopenings, in-person schooling arousing more questions than answers, vaccine allocation bringing its own set of problems, and travel restrictions tightening, the next twelve months may seem like a scary and confusing time.
After a year of severe mental anguish from the onslaught of the virus, the future remains in question. Countries and localities are likely to reverse the changes they’ve implemented over the past year, though some changes regarding human contact are likely to be permanent. What doesn’t remain in question, however, is how much people won’t take a return to normal for granted.
“In a post-COVID-19 world, I expect people to value physical and social interaction much more,” Sandhu said. “I feel as though people will understand the importance of others in their lives.”